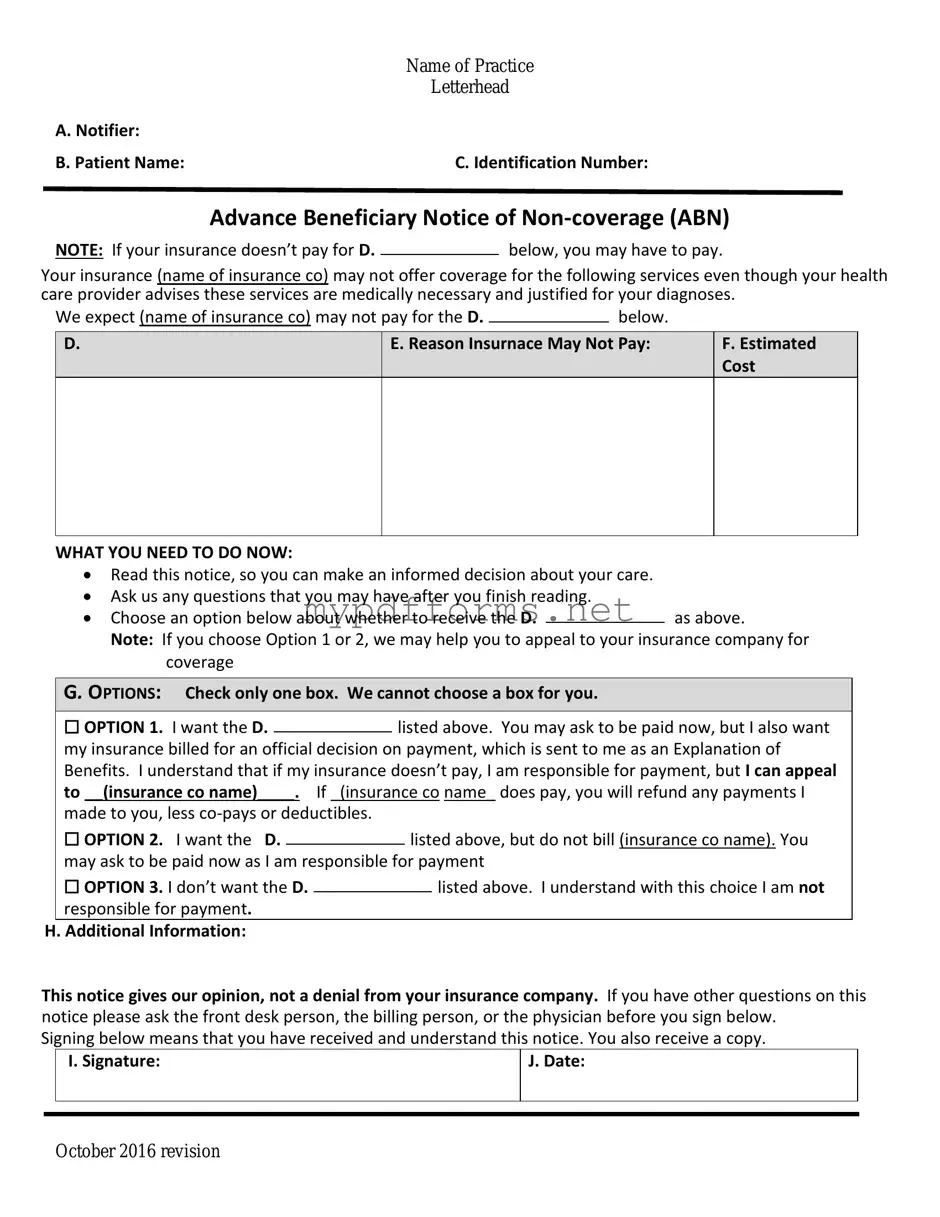
Get Advance Beneficiary Notice of Non-coverage Form in PDF
The Advance Beneficiary Notice of Non-coverage (ABN) is a crucial document that notifies Medicare beneficiaries when a service may not be covered by Medicare. This form helps patients understand their financial responsibilities before receiving certain medical services. To ensure you are informed about potential costs, consider filling out the ABN form by clicking the button below.
Modify Document Here
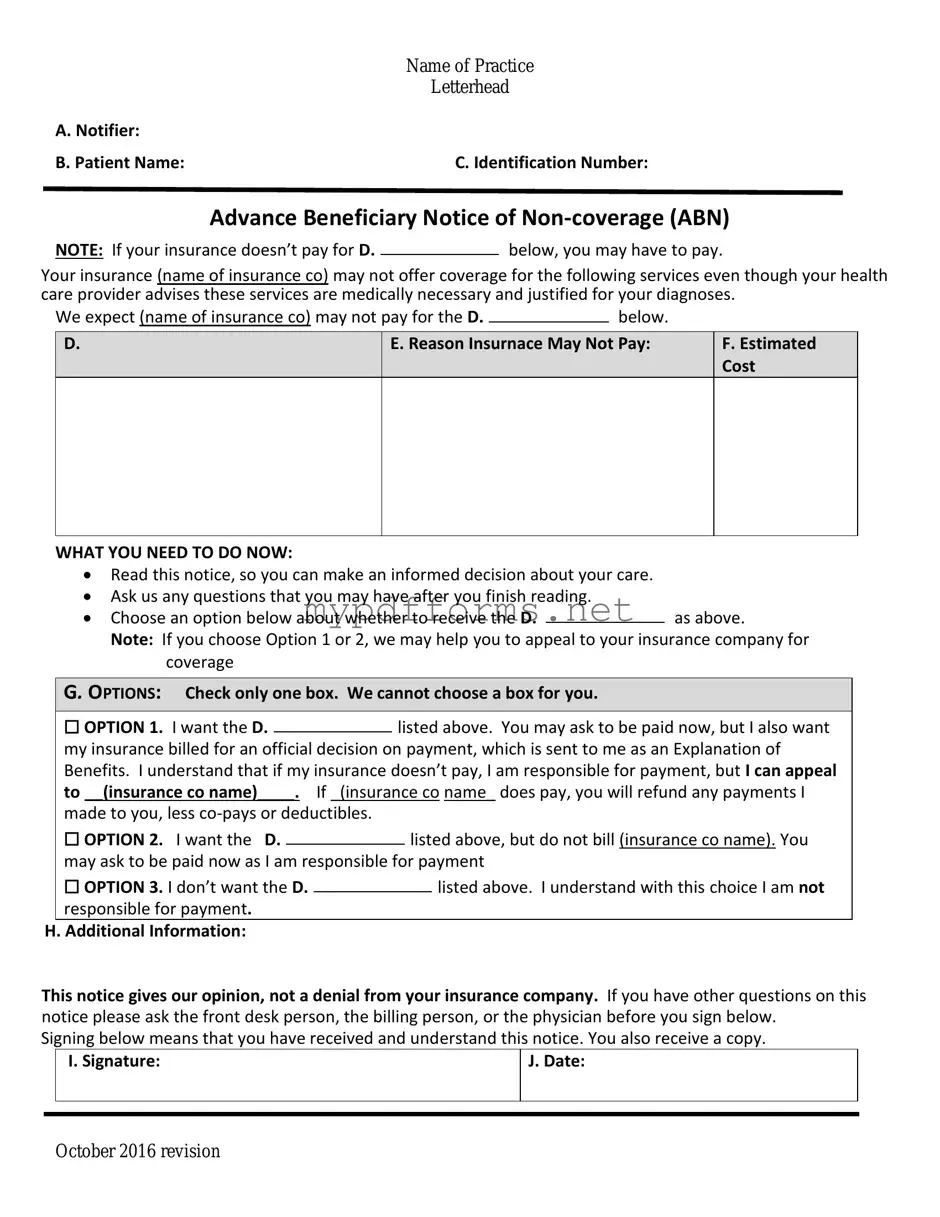
Get Advance Beneficiary Notice of Non-coverage Form in PDF
Modify Document Here
Modify Document Here
or
⇓ PDF
Need to check this off quickly?
Edit and complete Advance Beneficiary Notice of Non-coverage online in just a few steps.