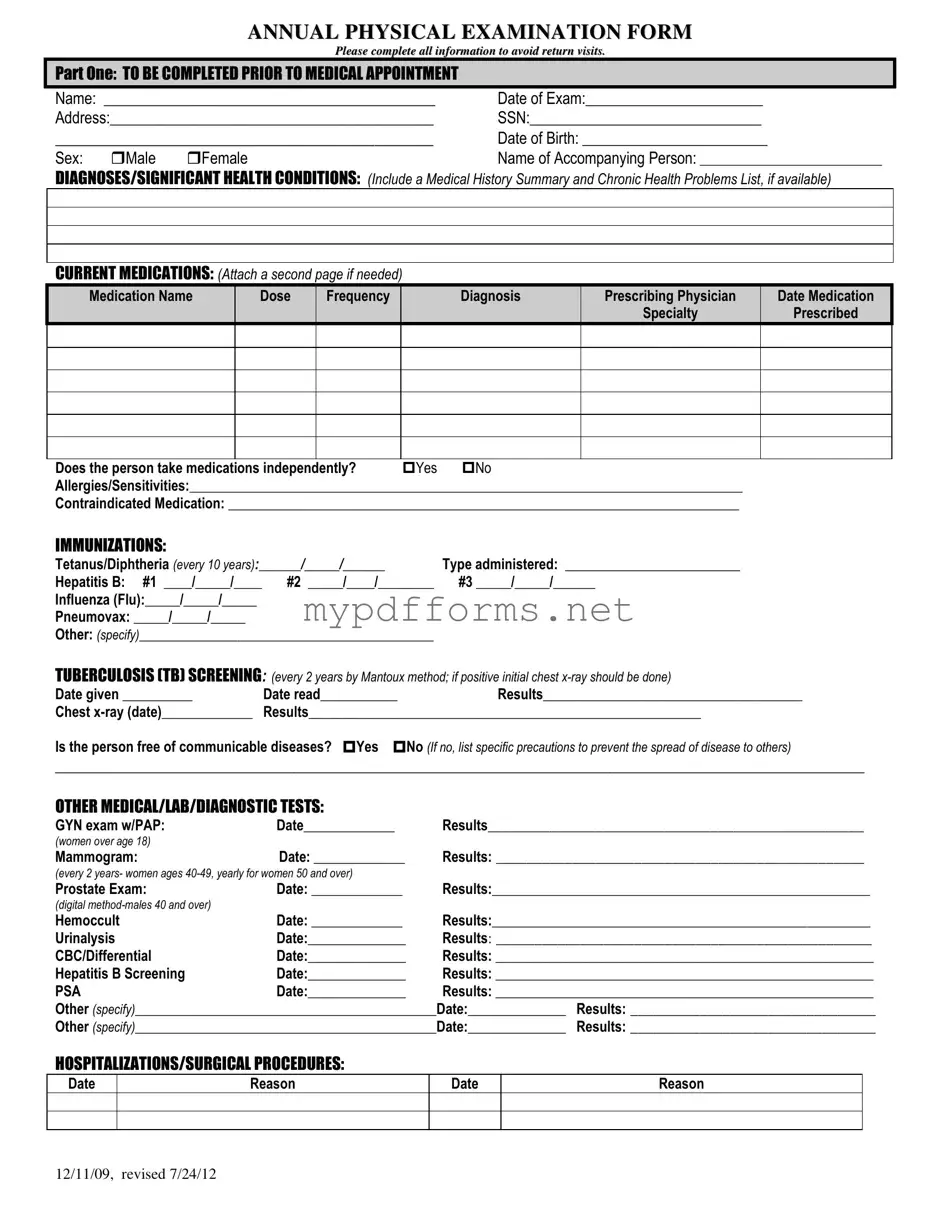
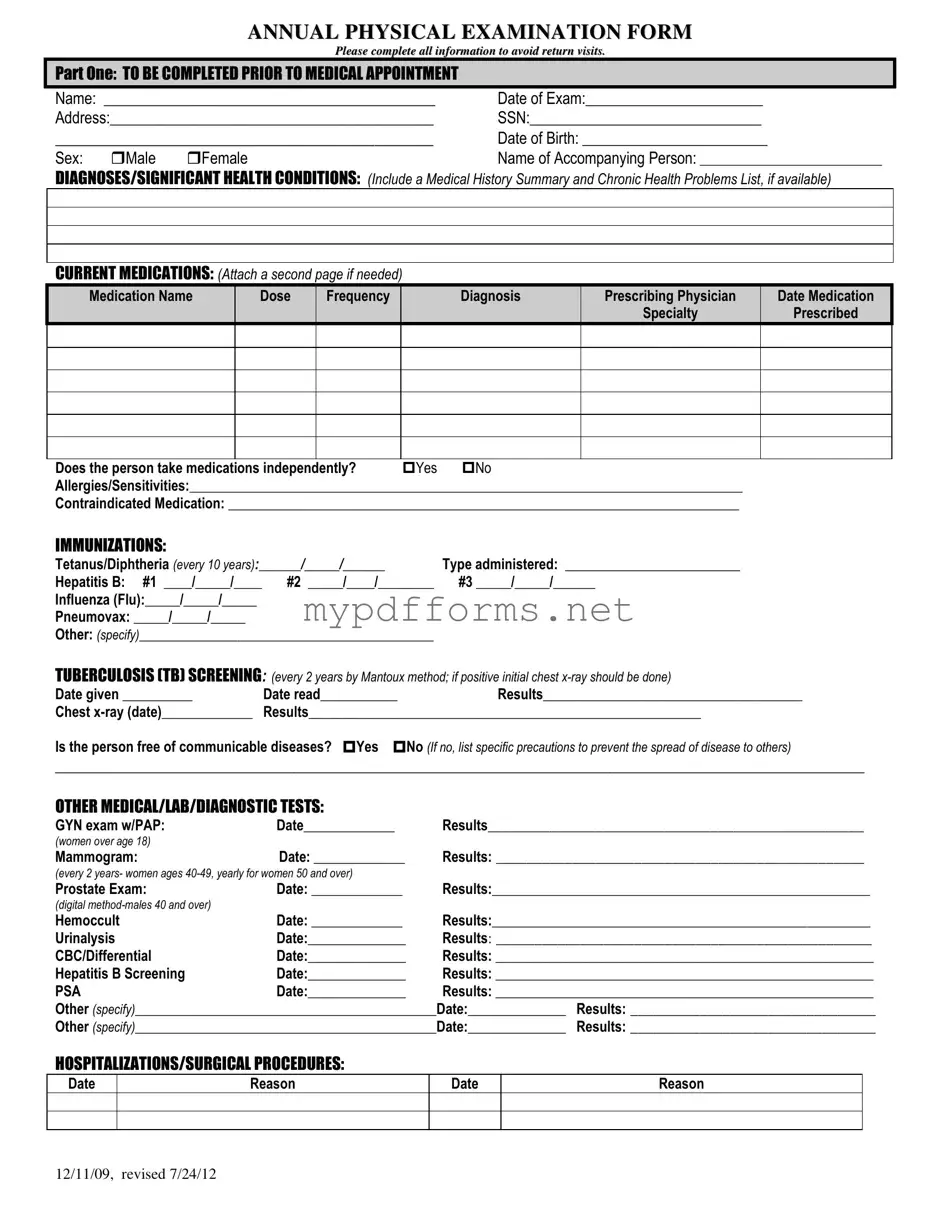
The Annual Physical Examination form shares similarities with the Medical History Form. Both documents aim to gather crucial information about a patient's past and current health status. While the Annual Physical Examination form focuses on current medications and specific health evaluations, the Medical History Form provides a broader overview of a patient's medical background, including previous illnesses, surgeries, and family health history. This comprehensive approach helps healthcare providers make informed decisions regarding diagnosis and treatment.
To ensure a well-structured workplace, employers should consider the essential guidelines outlined in the Employee Handbook, which can be accessed through the Illinois Forms. This document serves as a critical tool for aligning expectations and fostering a clear understanding of company policies and procedures.
Another document that resembles the Annual Physical Examination form is the Immunization Record. This record specifically tracks vaccinations received by an individual over time. Just like the Annual Physical Examination form, it requires precise dates and types of immunizations administered. Both documents play a vital role in ensuring that individuals are up-to-date with necessary vaccinations, which is essential for public health and individual protection against preventable diseases.
The Health Risk Assessment (HRA) is also similar to the Annual Physical Examination form. An HRA typically includes questions about lifestyle choices, medical history, and health screenings. Like the Annual Physical Examination form, it aims to identify potential health risks and encourage preventive measures. Both documents serve as tools for healthcare providers to assess an individual's overall health and recommend necessary interventions.
Additionally, the Consent for Treatment form bears resemblance to the Annual Physical Examination form. While the latter collects health information, the Consent for Treatment form focuses on obtaining permission from patients before they receive medical care. Both documents are critical in the healthcare process, ensuring that patients are informed and consenting to their treatment plans. This fosters a sense of trust and transparency between the patient and the healthcare provider.
The Patient Intake Form is another document akin to the Annual Physical Examination form. This form is often filled out by patients before their first visit to a healthcare provider. It gathers essential information about the patient’s health history, medications, and allergies, much like the Annual Physical Examination form. Both documents facilitate a comprehensive understanding of the patient’s health, enabling providers to tailor their care accordingly.
Lastly, the Laboratory Test Requisition form is similar in purpose to the Annual Physical Examination form. This requisition form is used to order specific lab tests based on the findings from a physical examination. Both documents emphasize the importance of monitoring health through various tests and evaluations. They work together to ensure that healthcare providers have the necessary information to diagnose and treat patients effectively.