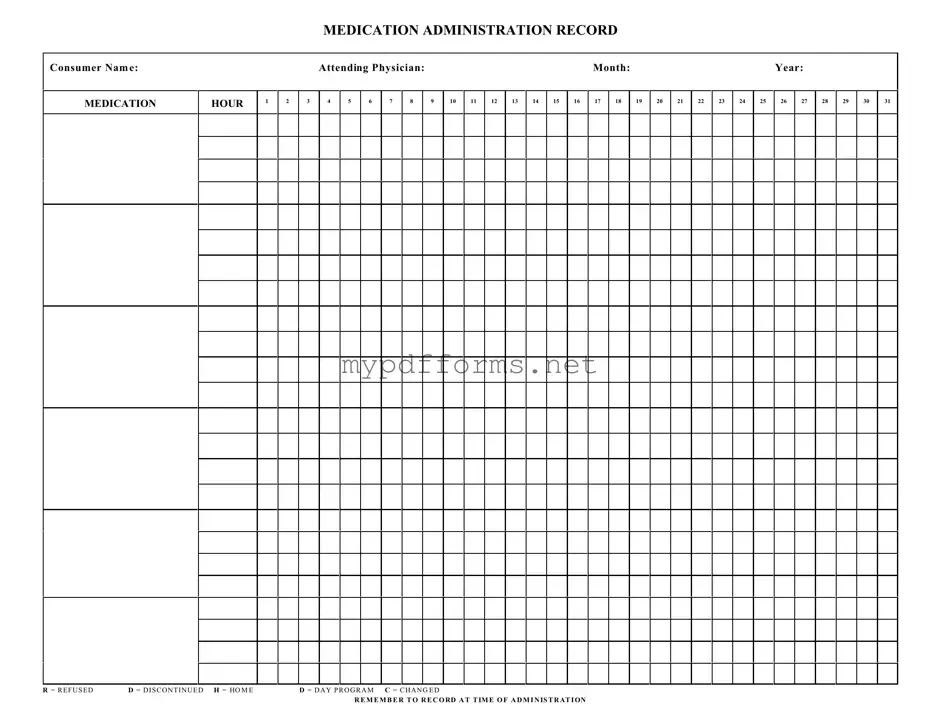
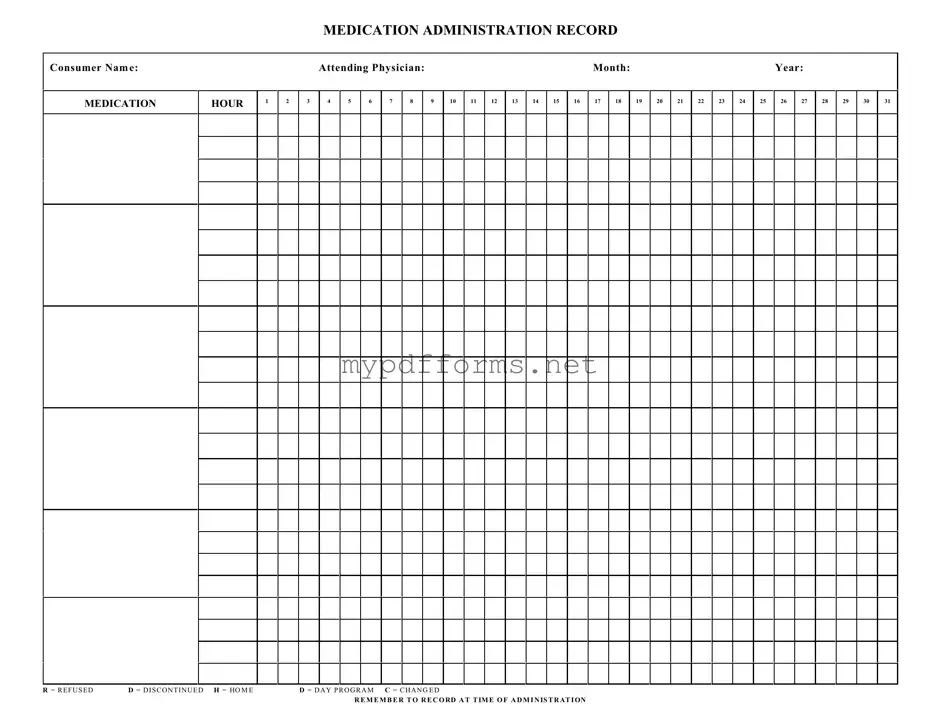
The Medication Administration Record (MAR) is similar to the Patient Medication Profile. Both documents provide essential information about a patient's medications. The Patient Medication Profile lists all medications prescribed to a patient, including dosages and administration routes. This profile is often used by healthcare providers to ensure that they have a comprehensive view of a patient's medication regimen. The MAR, on the other hand, focuses on the actual administration of those medications, documenting when and how each medication is given. This helps to track adherence and monitor any potential issues in real-time.
Another document that shares similarities with the MAR is the Medication Reconciliation Form. This form is used to compare a patient's current medications with those prescribed during a healthcare transition, such as a hospital discharge. Like the MAR, the Medication Reconciliation Form aims to prevent medication errors and ensure continuity of care. Both documents require accurate and up-to-date information to be effective, and they play a crucial role in patient safety by identifying discrepancies in medication regimens.
The Illinois Application for Firearm Control Card is a critical document for those seeking to carry firearms professionally, ensuring that applicants meet necessary criteria such as age and background checks. To facilitate the process effectively, it is essential to utilize the appropriate resources for obtaining this form, including Illinois Forms, which provides guidance on completing the application accurately. By following the correct procedures, individuals can ensure compliance with state regulations while pursuing their licensure to carry firearms in their respective professions.
The Treatment Administration Record (TAR) is another document akin to the MAR. While the MAR specifically focuses on medications, the TAR encompasses a broader range of treatments, including therapies and interventions. Both documents serve to track the administration of prescribed treatments and ensure that patients receive their care as intended. The TAR may also include notes on the patient's response to treatment, which can be valuable for ongoing care decisions.
The Care Plan is also similar to the MAR in that it outlines the specific interventions and medications a patient requires. The Care Plan is a comprehensive document that details the overall strategy for a patient's care, including goals and expected outcomes. In contrast, the MAR is more focused on the execution of those plans, recording the actual administration of medications. Both documents work together to ensure that healthcare providers are aligned in their approach to patient care.
The Incident Report shares some similarities with the MAR in terms of documentation. While the MAR tracks medication administration, the Incident Report records any adverse events or errors related to medication use. Both documents are crucial for maintaining patient safety and quality of care. They provide a mechanism for healthcare providers to learn from errors and improve practices, although they serve different purposes in the overall care process.
Lastly, the Nursing Notes can be compared to the MAR. Nursing Notes document a patient's condition and any care provided, including medication administration. While the MAR is specifically focused on medications and their administration, Nursing Notes provide a broader context of the patient's health status and care interventions. Together, these documents create a comprehensive picture of the patient's care, allowing healthcare providers to make informed decisions.