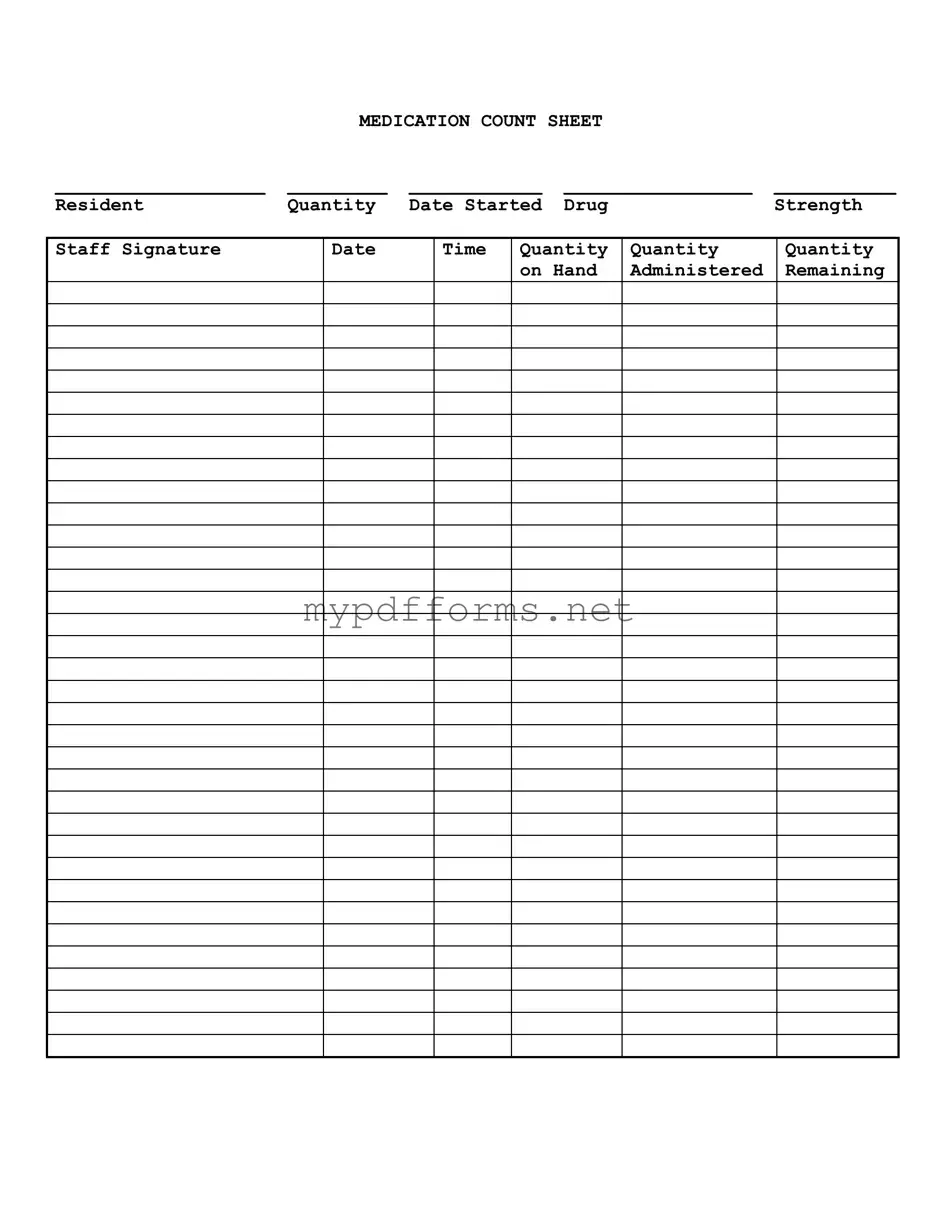
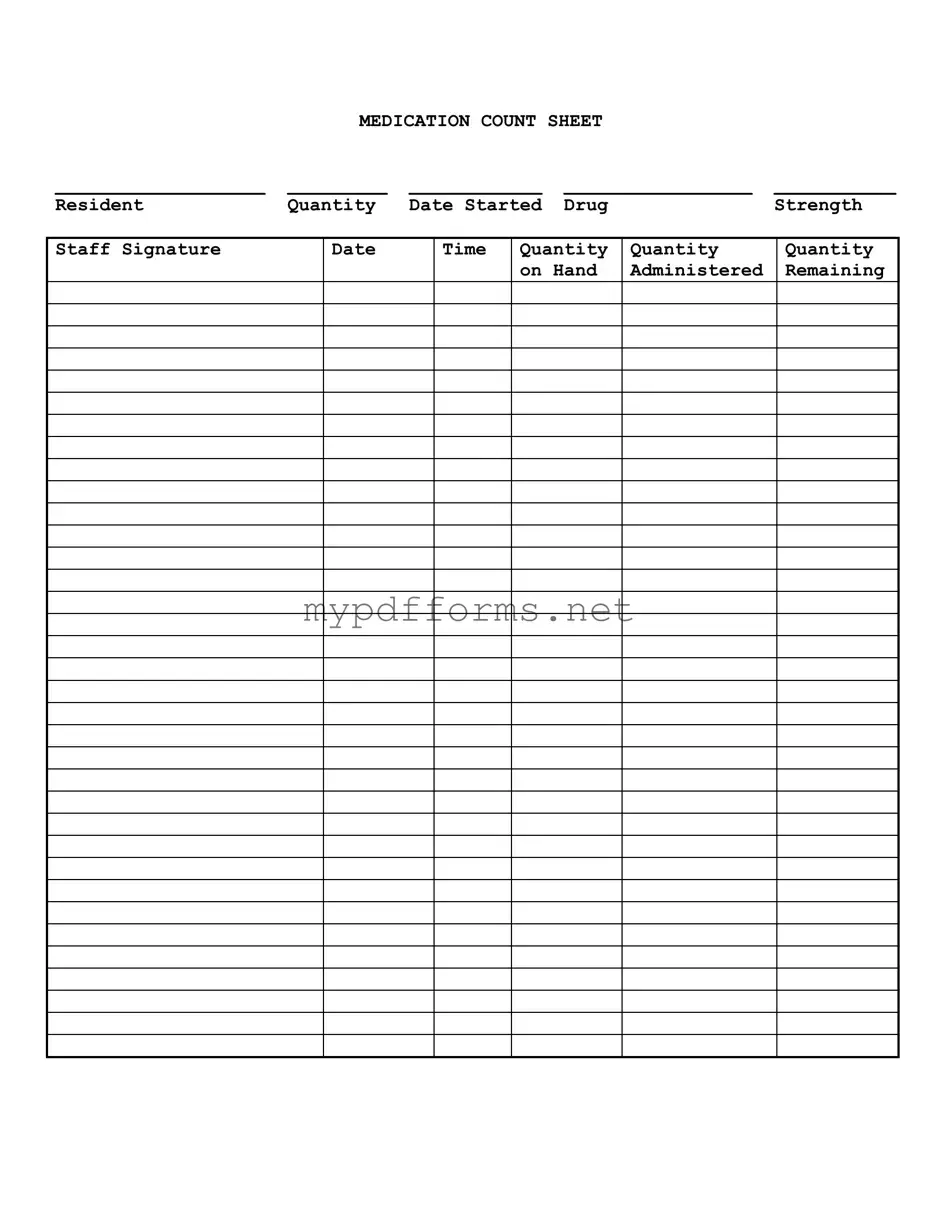
The Medication Administration Record (MAR) is a crucial document in healthcare settings. It tracks the administration of medications to patients. Similar to the Medication Count Sheet, it includes details such as the drug name, dosage, and administration times. Both documents ensure accountability and help prevent medication errors. Staff members must sign the MAR after administering each dose, reinforcing the importance of accurate record-keeping.
The Medication Reconciliation Form serves a different purpose but shares the goal of ensuring patient safety. This form is used to compare a patient’s medication orders to all medications the patient has been taking. Like the Medication Count Sheet, it requires careful attention to detail. Both documents aim to maintain accurate medication records, thereby reducing the risk of adverse drug interactions.
The Inventory Management Log is another similar document. It tracks the quantity of medications on hand in a facility. This log ensures that there are sufficient supplies available for patient care. Similar to the Medication Count Sheet, it records quantities and requires staff signatures. Both documents emphasize the importance of monitoring medication levels to avoid shortages.
Understanding the importance of documentation in healthcare can't be overstated, as accurate records are essential for maintaining patient safety and effective care. In this context, resources such as californiapdffoms.com provide helpful information on various forms, including those related to vehicle transactions, which can be just as critical in ensuring transparency and accountability within that domain.
The Controlled Substance Log is specifically designed for tracking controlled substances. It records the receipt, administration, and disposal of these medications. This log shares similarities with the Medication Count Sheet in that it requires detailed entries about drug quantities and staff signatures. Both documents are critical for compliance with regulations governing the handling of medications.
The Patient Medication History Form is used to document a patient’s past and current medications. This form is essential for understanding a patient’s treatment history. It parallels the Medication Count Sheet in that both require precise information about medications. Accurate medication histories can prevent potential conflicts and ensure that the patient's treatment plan is safe and effective.
The Medication Incident Report documents any adverse drug events or medication errors. While its primary focus is on incidents rather than routine administration, it still requires detailed information about the medications involved. Similar to the Medication Count Sheet, it emphasizes the importance of thorough documentation. Both documents play a role in improving medication safety practices within healthcare settings.
The Drug Utilization Review (DUR) form assesses the appropriateness of prescribed medications. This form evaluates whether the medications are being used effectively and safely. Like the Medication Count Sheet, it requires careful analysis and documentation. Both forms are integral to ensuring that patients receive optimal care while minimizing risks associated with medication use.
The Prescription Order Form is a document used to communicate medication orders from healthcare providers to pharmacies. It includes essential details such as drug name, dosage, and frequency. This form is similar to the Medication Count Sheet in that both require clear and accurate information to ensure proper medication management. Both documents are vital for maintaining continuity of care and preventing medication errors.
The Treatment Administration Record (TAR) is used to document all treatments administered to a patient, including medications. It contains similar information to the Medication Count Sheet, such as the date, time, and quantity of medications administered. Both documents are essential for tracking patient care and ensuring compliance with treatment protocols.