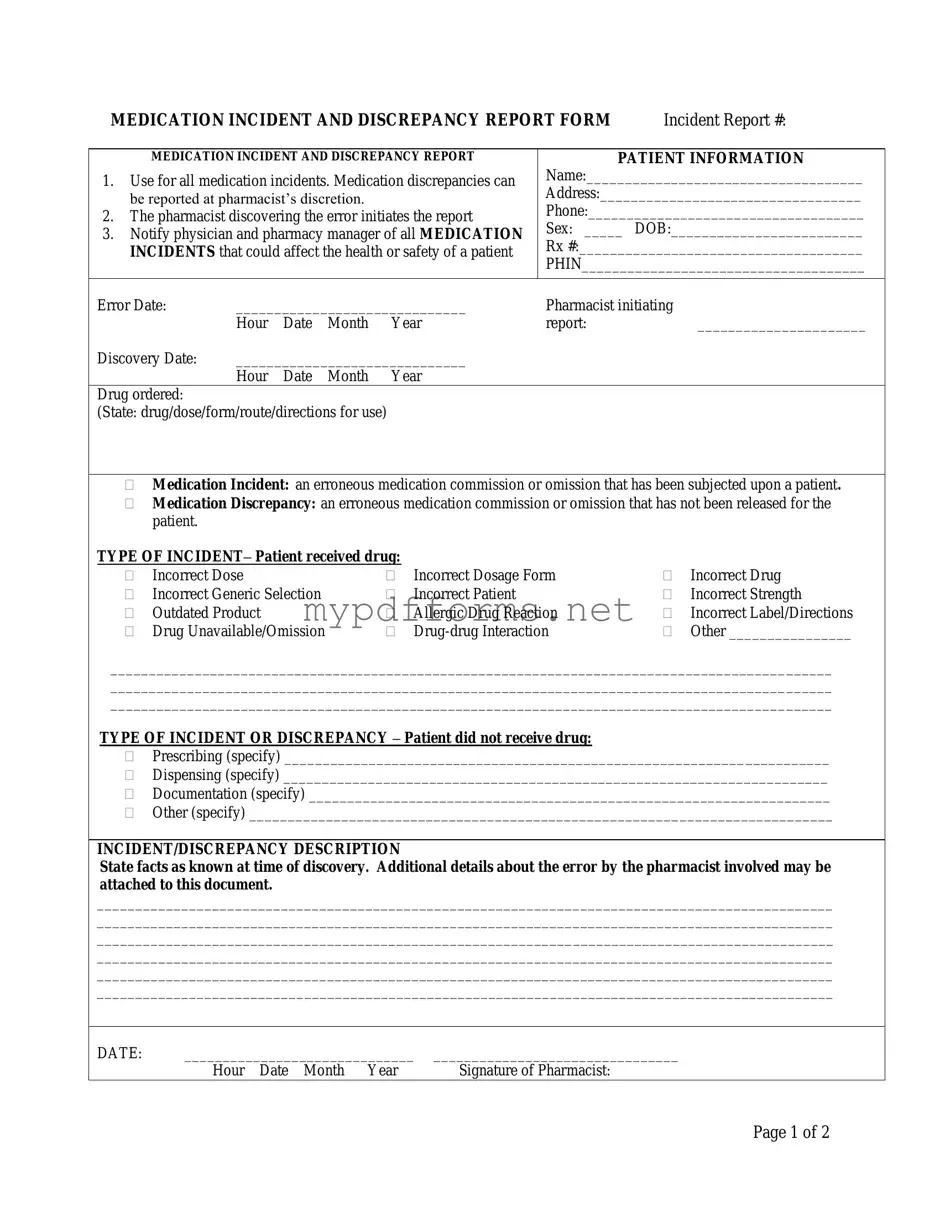
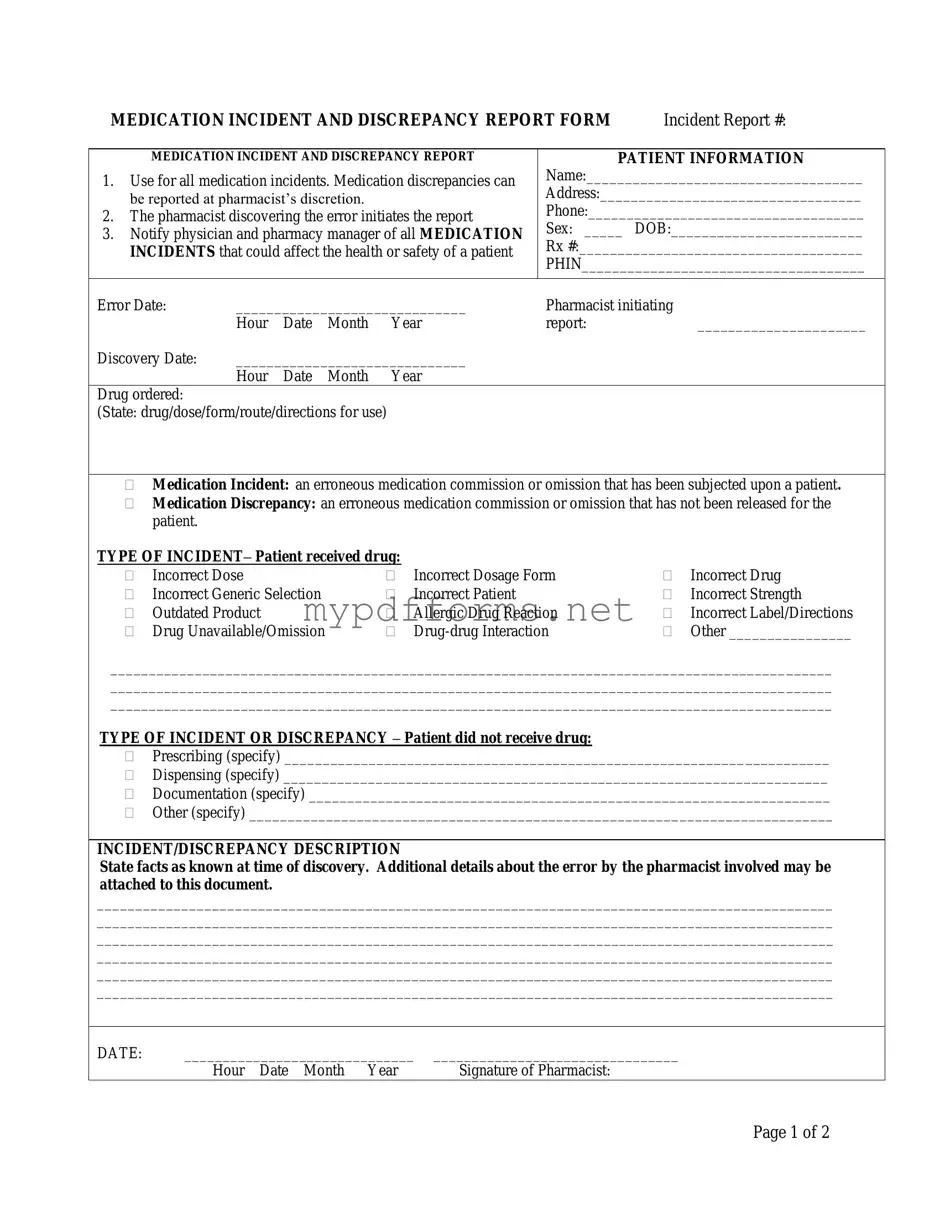
The Medication Error form shares similarities with the Incident Report form, which is commonly used across various industries, including healthcare. Both documents aim to document and analyze events that deviate from standard procedures, ultimately to enhance safety and prevent future occurrences. The Incident Report form captures essential details about the event, including the date, time, individuals involved, and a description of the incident. This information is crucial for identifying patterns and implementing corrective actions, just as it is in the Medication Error form.
Another document akin to the Medication Error form is the Adverse Event Report. This report specifically focuses on incidents where a patient experiences harm due to medical care or treatment. Like the Medication Error form, it requires detailed information about the event, including patient demographics and the nature of the adverse event. Both documents emphasize the importance of notifying relevant parties, such as healthcare providers and management, to ensure patient safety and improve care protocols.
The Root Cause Analysis (RCA) report is another document that aligns closely with the Medication Error form. An RCA investigates the underlying reasons for an incident, aiming to identify systemic issues rather than blaming individuals. Similar to the Medication Error form, it collects data about the event and involves input from various stakeholders. Both documents seek to promote learning and improvement within healthcare settings, ensuring that errors are addressed comprehensively.
The Quality Assurance (QA) report also bears resemblance to the Medication Error form. QA reports are used to evaluate the quality of care provided in healthcare facilities, focusing on compliance with established standards. Both forms require the collection of data related to incidents, including details about contributing factors and outcomes. The goal is to enhance the overall quality of care and minimize risks, making them essential tools for healthcare professionals.
The Patient Safety Report is another document that parallels the Medication Error form. This report is designed to capture safety-related incidents and near misses within a healthcare setting. Like the Medication Error form, it emphasizes the importance of reporting and analyzing incidents to prevent future occurrences. Both documents serve as critical components in fostering a culture of safety and accountability among healthcare providers.
Incident Command System (ICS) forms, used in emergency response situations, also share similarities with the Medication Error form. Both documents require clear and concise reporting of incidents, including essential details about the situation and the individuals involved. The ICS forms focus on coordinating responses to emergencies, while the Medication Error form aims to address medication-related incidents. However, both emphasize communication and documentation to ensure effective resolution and learning.
Understanding the importance of documentation in healthcare goes beyond just the Medication Error form. Various reports like the Quality Assurance Report and the Adverse Drug Reaction Report also play pivotal roles in ensuring patient safety and optimizing care. For those involved in property transactions, similar principles apply when utilizing legal documents such as the quitclaimdocs.com/fillable-michigan-quitclaim-deed/, which facilitates the transfer of property ownership while omitting title guarantees, thereby streamlining real estate processes.
The Risk Management Report is another document that aligns with the Medication Error form. This report focuses on identifying, assessing, and mitigating risks within healthcare organizations. Both documents require detailed descriptions of incidents, contributing factors, and outcomes. By analyzing this information, healthcare organizations can develop strategies to reduce risks and improve patient safety, thus reinforcing the purpose of the Medication Error form.
Lastly, the Clinical Incident Report is similar to the Medication Error form in that it documents clinical incidents that may affect patient care. This report collects information about the event, including the nature of the incident and the individuals involved. Both forms aim to analyze incidents thoroughly, ensuring that lessons learned are integrated into practice to improve patient outcomes and safety.