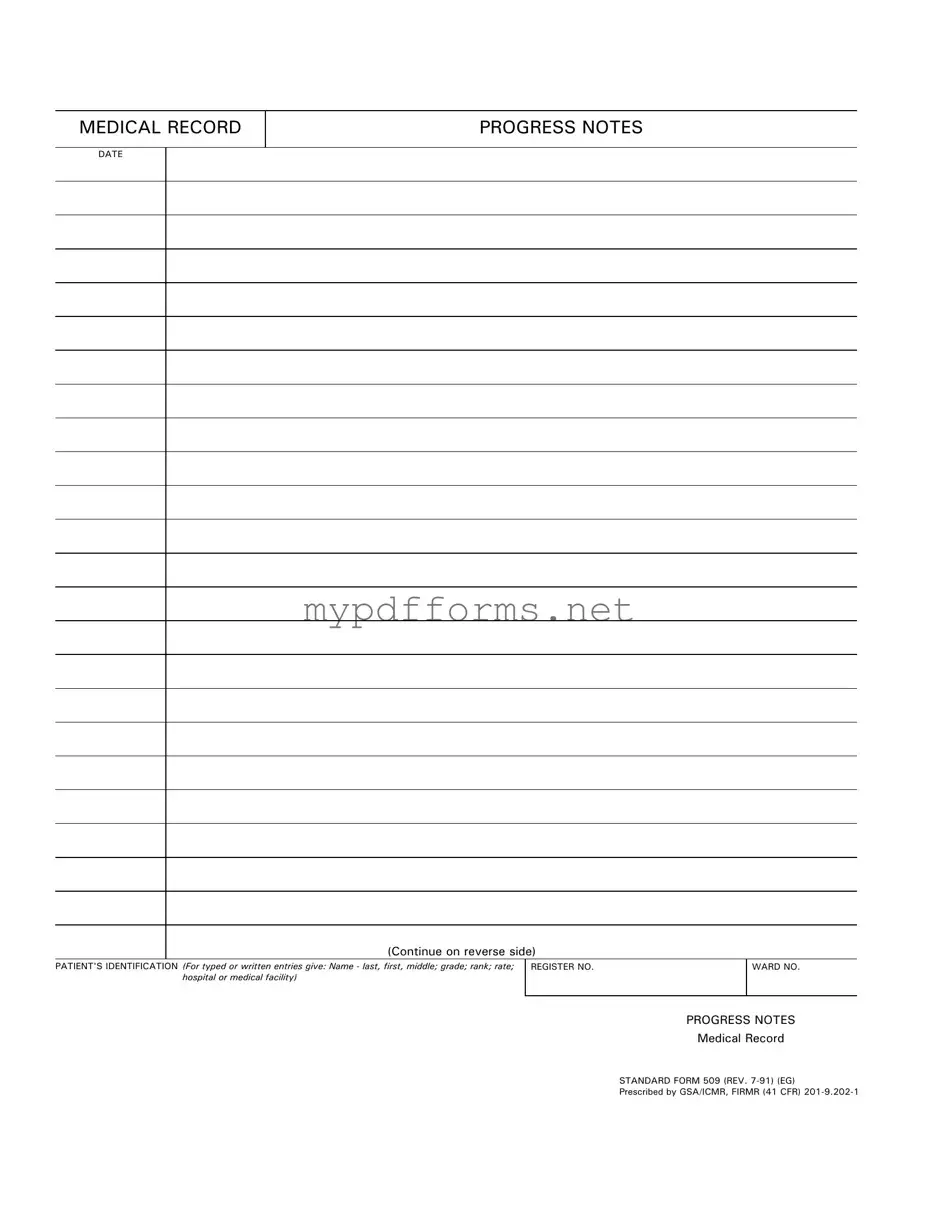
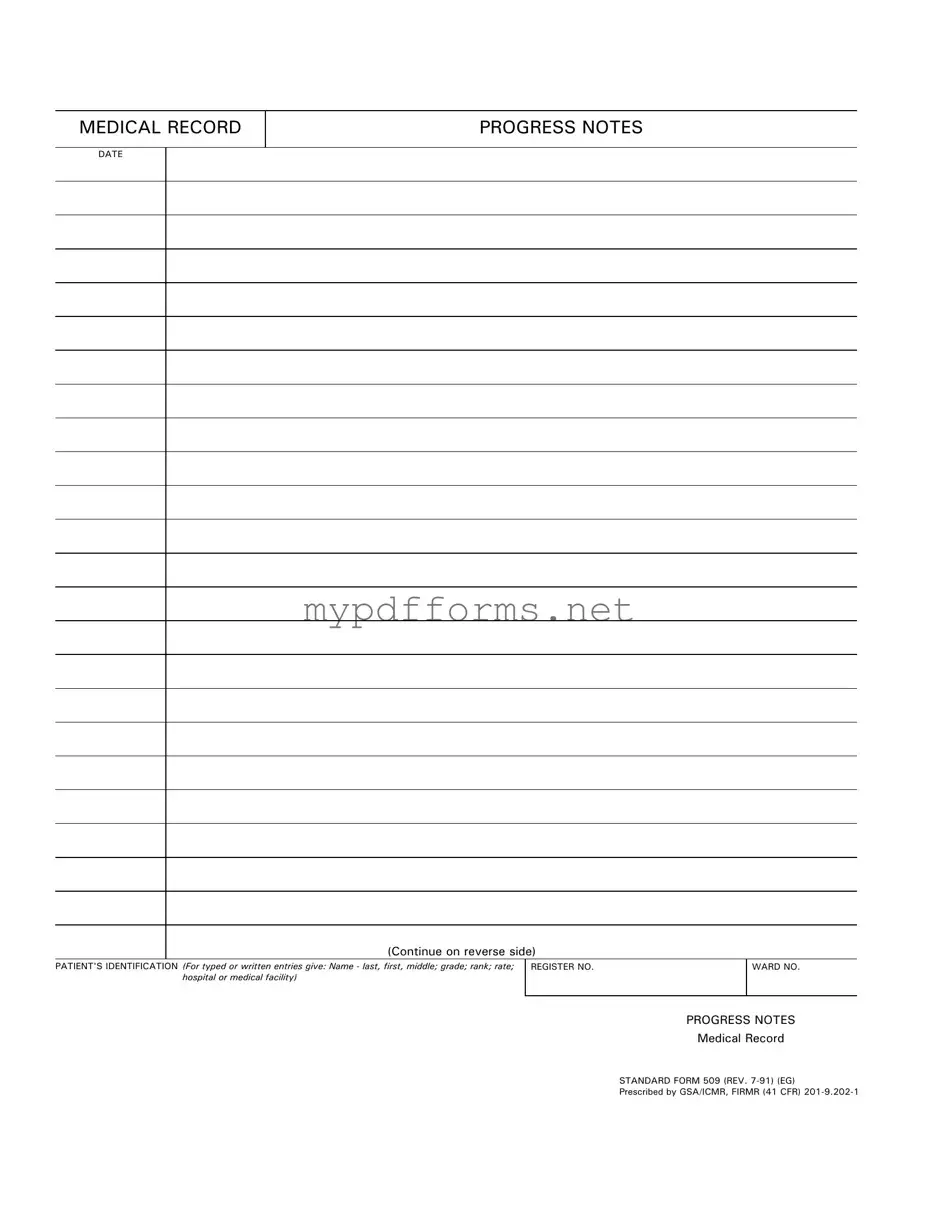
The Progress Notes form bears similarities to the Patient Encounter Form, which is often used in healthcare settings to document a patient's visit. Both forms serve as a record of the patient's condition and the care provided during a specific encounter. While the Progress Notes focus more on the ongoing treatment and observations made by healthcare professionals, the Patient Encounter Form typically includes details such as the reason for the visit, vital signs, and any immediate assessments. Together, these documents help create a comprehensive view of the patient's healthcare journey.
In the context of estate planning, a Last Will and Testament form in Illinois is essential for ensuring that your wishes regarding asset distribution and care for dependents are fulfilled after your passing. This legal document also designates an executor to manage your estate throughout the process. To make the process easier and to ensure that your wishes are honored legally, you may want to explore resources available through Illinois Forms, which provide the necessary templates and guidance for completing your Last Will and Testament effectively.
Another document comparable to the Progress Notes is the Treatment Plan. This document outlines the specific strategies and interventions designed to address a patient's health issues. Like Progress Notes, the Treatment Plan is used by healthcare providers to track a patient's progress over time. However, the Treatment Plan is more focused on future actions and goals, while Progress Notes record the actual observations and changes that occur during each visit. Both documents are essential for ensuring continuity of care and effective communication among medical staff.
The Clinical Summary is also similar to the Progress Notes form. This document provides a concise overview of a patient's medical history, current health status, and any recent treatments. While Progress Notes detail the ongoing observations and interactions with the patient, the Clinical Summary synthesizes this information into a broader context. It serves as a quick reference for healthcare providers, allowing them to understand a patient's overall condition and treatment history at a glance, thereby facilitating informed decision-making.
Lastly, the Discharge Summary shares similarities with Progress Notes, as both documents are integral to patient care continuity. The Discharge Summary is created at the end of a patient’s treatment, summarizing their hospital stay, treatments received, and recommendations for post-discharge care. Progress Notes, on the other hand, are updated throughout the treatment process. Both documents aim to provide a clear and comprehensive account of a patient's care, ensuring that all healthcare providers involved in the patient's ongoing treatment are well-informed and aligned in their approach.