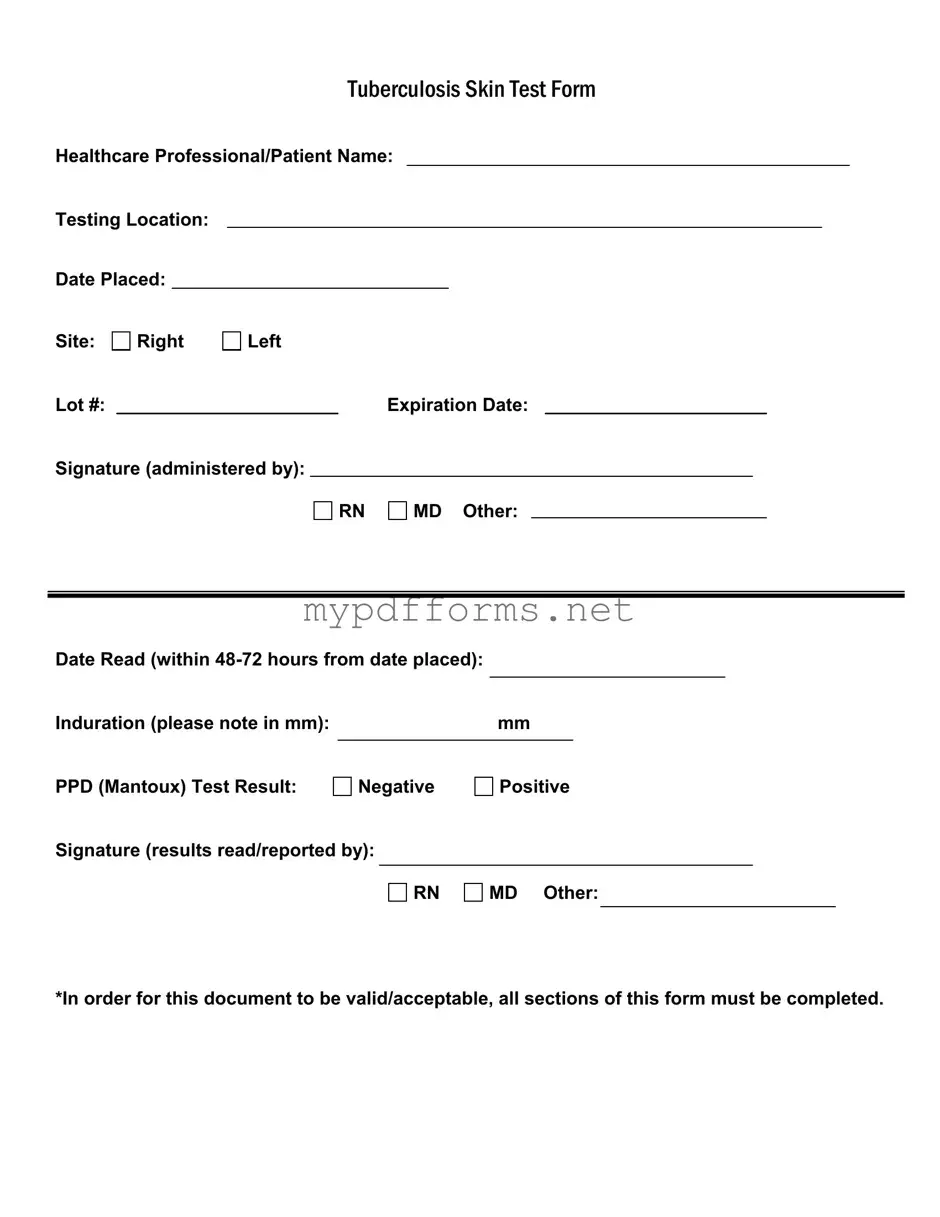
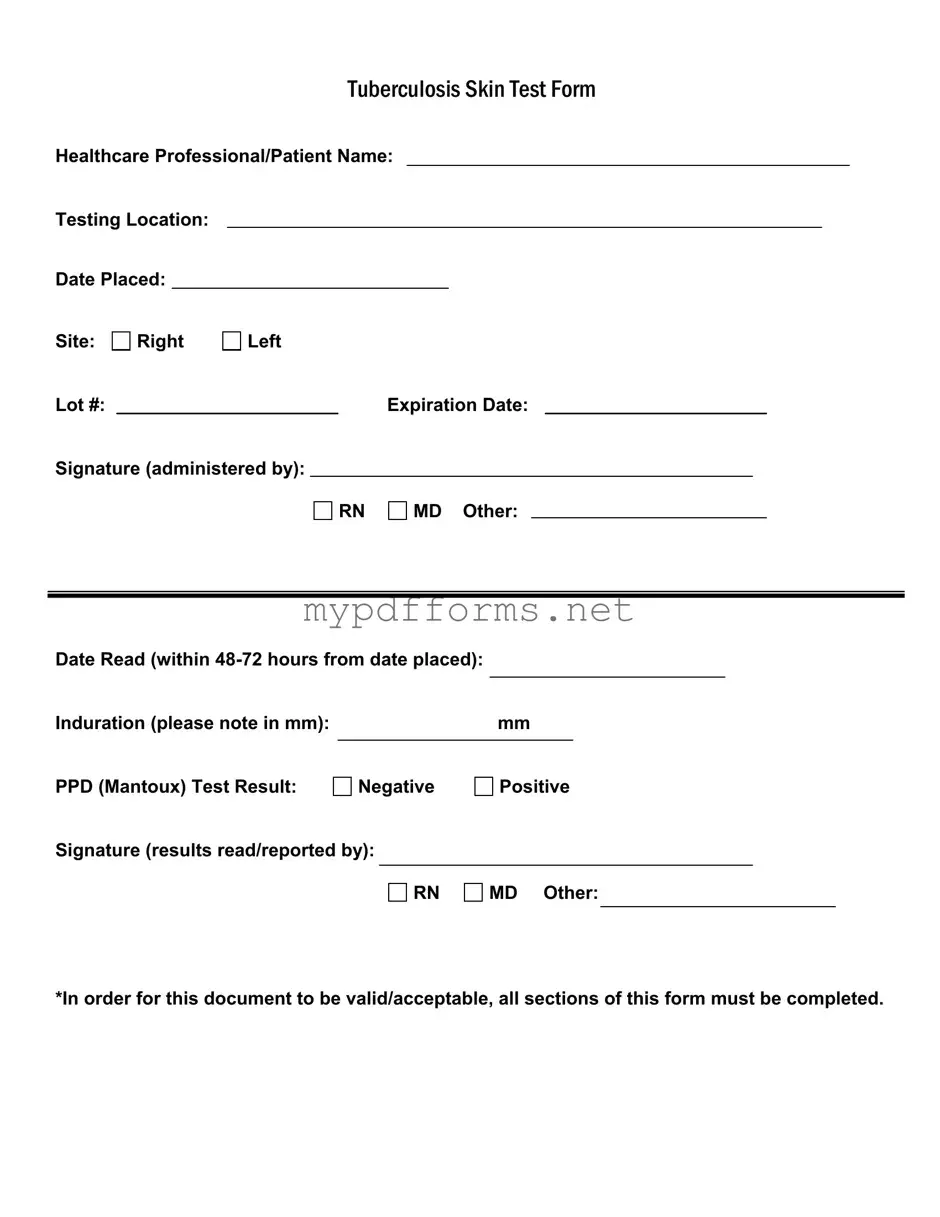
The TB Test form is similar to the Immunization Record form. Both documents serve as official records of a person's health status regarding communicable diseases. The Immunization Record includes details such as the type of vaccine administered, the date of administration, and the healthcare provider's signature. Like the TB Test form, it requires accurate completion and often serves as proof for schools, employers, or travel requirements.
Another comparable document is the Health Screening Form. This form collects essential health information from individuals, including previous medical history and current health status. Both forms are crucial for assessing a person’s health risks and ensuring that they meet specific health standards for employment or educational purposes. They also require signatures from healthcare professionals to validate the information provided.
The Medical Clearance Form is also similar. This document confirms that an individual is fit for a particular activity, such as sports or work. It includes details about medical evaluations and any necessary tests, much like the TB Test form. Both documents are signed by a healthcare provider, ensuring that the individual meets the required health criteria before participating in certain activities.
Additionally, the Physical Examination Form shares similarities with the TB Test form. It documents the results of a physical exam, including vital signs and any health concerns. Like the TB Test, it requires a healthcare professional's signature and is often used to verify that an individual is in good health for school or employment. Both forms aim to protect public health by ensuring individuals do not pose a risk to others.
When considering documentation for motorcycle transactions, the Minnesota Motorcycle Bill of Sale form is particularly noteworthy, as it plays a vital role in ensuring that ownership is transferred legally and efficiently. This form outlines important details about the motorcycle and the parties involved, much like other essential medical documents that require comprehensive completion. For those looking to create or fill out this form, further information can be found at https://motorcyclebillofsale.com/free-minnesota-motorcycle-bill-of-sale.
Lastly, the Consent for Treatment Form is another document that aligns with the TB Test form. This form is used to obtain permission from a patient before administering a test or treatment. Both documents require clear and complete information, including signatures from both the patient and the healthcare provider. They ensure that patients are informed about the procedures they undergo and that their consent is documented properly.